Lisa Montel, Anuj Kapilashrami, Michel P. Coleman, and Claudia Allemani |*|
Abstract
The UK’s response to COVID-19 has been widely criticized by scientists and the public. According to EuroMOMO, a European mortality monitoring initiative, the excess mortality that may be attributable to COVID-19 in England is one of the highest in Europe, second only to Spain. While critiqued from a public health perspective, much less attention is given to the implications of the pandemic outbreak for the right to health as defined under international human rights law and ratified by member states. Using the UK as a case study, we examine critically the extent to which the government’s response to COVID-19 complied with the legal framework of the right to health. We review further key states’ obligations on the right to health and assess its suitability in times of pandemic. Finally, we offer some recommendations for an update of the right to health.
Introduction
On April 22, 2020, the European Committee of Social Rights, the body responsible for overseeing the implementation of the European Social Charter, issued its Statement of Interpretation on the Right to Protection of Health in Times of Pandemic. [1] This statement emphasizes the interrelation of the right to protection of health with other rights enshrined in the European Social Charter, such as the right to social and medical assistance, the right to housing, the right to freedom from poverty and social exclusion, and the right to safe and healthy working conditions. States’ obligations to realize further the right to health in response to COVID-19 were also addressed by UK experts in a submission to the Parliamentary Joint Committee of Human Rights in July 2020. [2] The submission includes recommendations for the protection of vulnerable groups, preparedness, essential medical goods, testing and tracing, lockdowns, vaccines, the right to access other health services, long-term care for COVID-19 patients, international cooperation, and accountability.
These statements show the importance of systematically applying the right to health to public health policies when addressing the COVID-19 pandemic. This has also been reiterated by the United Nations (UN), the World Health Organization (WHO), and the UN Special Rapporteur on the right to health. [3]
The UK’s response to the pandemic has been widely criticized by experts in human rights and the public health community. [4] Analyses from EuroMOMO, a European mortality monitoring project, show that England has the second excess mortality in Europe. [5] This, despite the fact that the UK is a signatory to several UN and regional treaties protecting the right to health, including the European Social Charter and the International Covenant on Economic, Social and Cultural Rights (ICESCR). [6]
In this context, we take the UK as a case study to evaluate its early response to the pandemic and to assess the extent to which it fulfilled its obligations arising from the right to health. We use the Committee on Economic, Social and Cultural Rights’ General Comment 14 as the legal reference to assess five of the UK’s core obligations arising from the right to health: (1) to ensure the right of access to health facilities, goods, and services on a non-discriminatory basis; (2) to ensure access to the minimum essential food; (3) to take measures to prevent, treat, and control epidemic and endemic diseases; (4) to provide education and access to information concerning health; and (5) to provide appropriate training for health personnel. [7] We choose to rely on General Comment 14 because, although not legally binding, it constitutes a global understanding of the normative content of the right to health. [8] We build on the analysis of General Comment 14 to reflect on the legal framework of the right to health and offer some recommendations to adapt it further to the context of pandemics.
This article contributes to the robust international legal framework for the right to health. So far, the literature has explored various areas, including health rights in HIV/AIDS and maternal health, as well as policy issues such as patent rights and access to medicines. To that effect, Covid-19 presents itself as another opportunity to examine and discuss the right to health in times of pandemic.
The UK and the right to health
The UK has signed and ratified both the 1961 European Social Charter and the 1966 ICESCR, which protect the right to health in their articles 11 and 12, respectively. [9] It is also a signatory to other UN treaties that protect the right to health of specific groups, including the Convention on the Elimination of All Forms of Discrimination against Women, the Convention on the Rights of Persons with Disabilities, and the Convention on the Rights of the Child. [10]
We assess the extent to which the UK respected its obligations under the right to health when it responded to the onset of the pandemic, from February to May 2020. This period was crucial for preparedness and the adoption of principles such as availability, accessibility, acceptability, and quality of health services, as well as non-discrimination, participation, and accountability of the state in its public health response.
During these four months, the government took decisions on triaging patients in primary health care, testing and tracing, the provision of essential medical goods and personal protective equipment (PPE), lockdown measures, and the communication of data on incidence and mortality for epidemiological research. All of these decisions had an impact on the right to health of its people, including their access to health services, equal access to treatment, the right to access health information, and the right to be treated for diseases other than COVID-19.
The right to health requires states to take positive action and engage their financial and human resources. As a result, they are subject to the principles of progressive realization and maximum available resources—in other words, states must take steps to realize the right to health gradually and continuously over time, and they must not take any retrogressive action. [11] To that effect, however, there are some core obligations that each state must fulfill immediately to realize the right to health, regardless of its economic and human resources. Such obligations are outlined by the Committee on Economic, Social and Cultural Rights in General Comment 14 (Box 1). [12] Because the core obligations must be applied immediately and are not subject to the availability of resources, we chose to assess the UK’s adherence to five of these obligations that we found relevant in the context of its early response to the pandemic.
The UK’s response to COVID-19
To tackle outbreaks of infectious diseases, WHO recommends containing their spread by testing persons for the presence of a disease, tracing their contacts, quarantining suspected cases, and treating confirmed cases. If the disease has spread in the community, the government must ensure that health facilities can cope with the patients who require hospital care. [13]
On December 31, 2019, WHO’s China Country Office received a report about an unknown virus behind a number of pneumonia cases in Wuhan. [14] On January 12, 2020, the Chinese government made the genetic sequence of the virus publicly available. [15] This was to facilitate international efforts to develop diagnostic tools, to speed up research for a vaccine, and to ensure preparedness in case of an outbreak. Meanwhile, the situation degraded rapidly, and on January 30, 2020, the WHO director-general declared a “Public Health Emergency of International Concern.” [16] WHO’s Emergency Committee issued temporary recommendations: “All countries should be prepared for containment, including active surveillance, early detection, isolation and case management, contact tracing and prevention of onward spread of 2019-nCoV infection, and to share full data with WHO.” [17] This coincided with the UK reporting its first lab-confirmed case of COVID-19. Figure 1 presents a timeline of key responses in the UK.
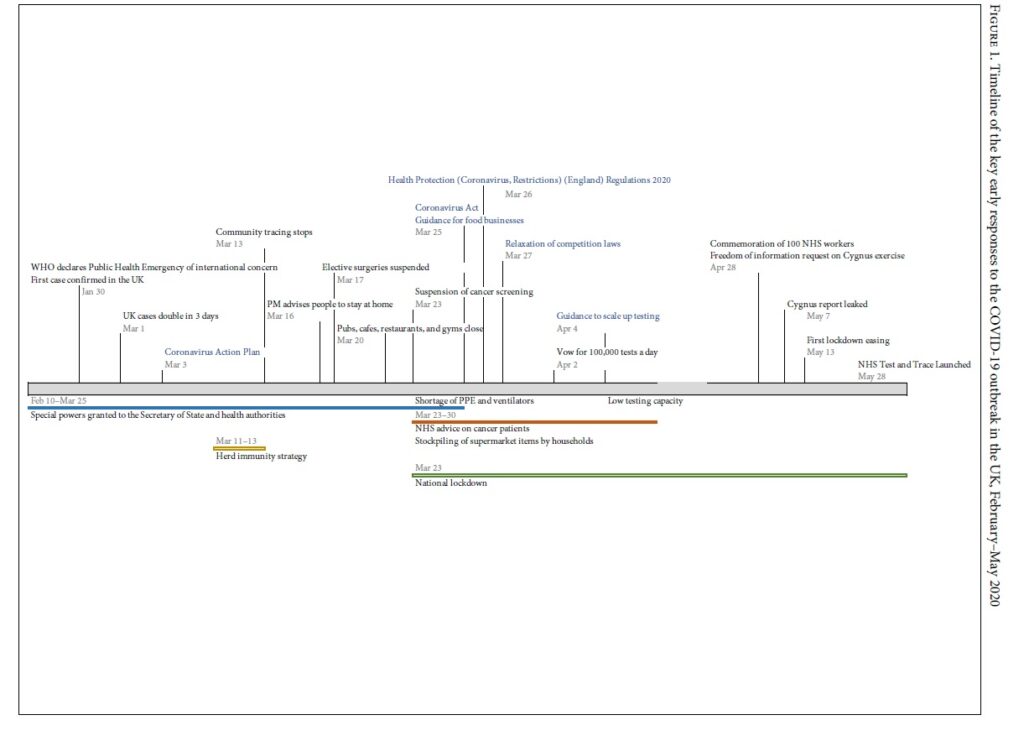 |
Obligation 1: Ensure the right of access to health facilities, goods, and services on a non-discriminatory basis, especially for vulnerable or marginalized groups
Ensuring non-discriminatory access to health care demands that attention be given to specific vulnerable groups. In the context of COVID-19, early analyses revealed that social inequalities exacerbate risks of COVID-19 and highlighted key vulnerable groups. These include elderly persons with chronic conditions, minority ethnic populations, persons from the lowest wealth quintile, and non-COVID patients with another serious illness. [18] The failure of the UK government to tackle these vulnerabilities and to make specific provisions for vulnerable groups resulted in higher case fatalities among Black, Asian, and Minority Ethnic (BAME) groups in comparison to white population in deprived regions as well as in care homes. [19] This marks a violation of their right to health.
Generally, access to primary health care in the UK was severely disrupted. From mid-March, general practices implemented triage by phone, thus limiting the number of patients allowed to visit their primary care physician in person or be referred to another health professional. [20] The health impacts on primary care disruption have yet to be estimated but will have mid- to long-term implications for the National Health Service (NHS), with some chronic conditions worsening, new conditions diagnosed too late, and referrals to special services such as cancer and mental health being postponed or canceled. Because of the long queuing time over the phone and the digitalization of health consultations, phone triages may be discriminatory toward poorer households whose phone contracts may limit communication time each month and toward older patients who may find the use of new technologies challenging.
Access to acute secondary care services was also severely affected. On March 17, 2020, hospitals were instructed to suspend all elective surgical procedures for at least three months. [21] NHS trusts were instructed to redesign their services to free up capacity for COVID-19 patients. [22] Yet it is estimated that 50% of elective procedures can inflict significant harm to the patient if postponed or canceled. [23]
Several guides were published by NHS England to propose a system of priority levels for surgical procedures for cancer patients. [24] On March 30, it advised maintaining cancer treatment during the COVID-19 response. [25] However, the non-compulsory nature of the document meant that the responsibility lay with local health trusts, which introduced inconsistency in implementation. [26] As a result, some high-risk cancer patients faced delays in their treatment.
In addition, national cancer screening was suspended to allow the deployment of frontline health workers for COVID-19. [27] The number of high-risk patients being referred by their general practitioner for a possible cancer diagnosis dropped by roughly 70% in Scotland and Northern Ireland. [28]
While the government prioritized the treatment of COVID-19 patients, it failed to ensure that other serious health conditions could be diagnosed and treated promptly. By publishing soft guidance for local NHS trusts, the state delegated its responsibility to ensure access to health services and facilities to everyone, which created inequalities in access between geographical regions.
Obligation 2: Ensure access to the minimum essential food
This obligation means that the government must take action, if necessary, to ensure that persons on a low-income or homeless have access, on a daily basis, to the minimum essential food that is nutritionally adequate and safe. [29]
On March 21–22, 2020, the weekend preceding the lockdown, many people rushed to supermarkets and started stockpiling supplies such as food and antibacterial handwash. In its official guidance, the UK government focused on food hygiene, social distancing, and employee sickness but did not include any advice for supermarkets on how to regulate the flow of supplies. [30] Nor did it advise citizens to shop responsibly. [31] As a result, the week running up to and the first few weeks of the lockdown witnessed a scarcity of fresh fruit, vegetables, milk, and bread in supermarkets. More affluent households were able to stockpile, while poorer households found themselves unable to procure essential items due to their scarcity.
The government appeared to leave the burden of decision-making to private actors—namely supermarkets—to ensure that there was an adequate food supply. Partial regulation was seen at some point, when the government relaxed competition laws to allow supermarkets to exchange otherwise competitively sensitive information. [32] The aim was to allow supermarkets to shift the priority from competing with one another toward ensuring that enough essential items would be available everywhere in the country. The Coronavirus Act 2020 on food supply provided only a monitoring power to the government through the requesting of information from businesses or persons working in the food industry. [33] One may argue that the state had a duty to regulate supermarkets in order to ensure the availability of food for the entire nation in these special circumstances.
The lack of strong government intervention meant that existing inequalities in access to food widened. People living on low wages or who had lost their job during the lockdown increased the demand on food banks. At the same time, donations to those foodbanks decreased because of stockpiling. Families relying on school meals for their children also found themselves in strenuous situations. [34] This represented a violation of the state’s core obligation to ensure access to minimum essential food and the right to food, as protected by article 11 of the ICESCR.
Obligation 3: Take measures to prevent, treat, and control epidemic and endemic diseases
A state can prevent and control an infectious disease by providing vaccination at the population level. With no vaccine available for the SARS-CoV-2 virus, states are left with the test-and-trace strategy, as well as scaling up their health care system’s capacity to treat new cases. [35]
On March 1, 2020, the UK recorded its highest surge in new cases, which represented a doubling of the number of cases in just three days. [36] The government had had one month since the WHO’s declaration of the “Public Health Emergency of International Concern” before that first surge in cases to prepare its response to the spread of the novel coronavirus. During this period, the official strategy was unclear, and communication to the public was inconsistent.
On March 3, 2020, the official strategy from the government’s Coronavirus Action Plan was to contain, delay, research, and mitigate. [37] However, in mid-March, the government contemplated achieving herd immunity by allowing a large proportion of its population to become infected and then recover. [38] At the time, estimates suggested that up to 260,000 deaths could have been expected. [39] This approach came under scrutiny for lack of evidence on immunity, and uncertainty around the epidemiology of the virus and the disease it causes.
Following substantial criticism from the scientific community at home and abroad, as well as media scrutiny, the government shifted its strategy on March 16. [40] People were strongly advised to stay at home, but the decision to travel to work remained with employers. Social venues remained open until March 20, and it was not mandatory for major events to be canceled. On March 23, a national lockdown was finally announced, and a few days later it went into effect. [41]
Although the government’s new strategy followed WHO’s advice, it came too late. [42] The incubation period for COVID-19 meant that the effect of the lockdown would be seen only after about two weeks. Meanwhile, the NHS was faced with a rapid increase in the number of patients who needed treatment in intensive care units, including artificial ventilation for lung failure.
Despite the government’s strategy to prioritize strengthening the capacity of the health care system and maintaining the functionality of tertiary services, it failed to equip health care workers adequately with PPE and to provide enough ventilators for seriously ill patients. [43] For instance, on March 17, the UK failed to take up an offer from the European Union to participate in a joint procurement call to buy ventilators for 25 member states. [44] Significant shortages in PPE also meant that NHS staff on the front lines were risking their lives. When NHS staff developed COVID-19 symptoms, they had to self-isolate for 14 days, thus reducing the workforce further. [45] The government also failed to enforce guidelines to reduce transmission to residents and workers in care homes, among whom the proportion of new cases and deaths was later shown to be much higher than in other population groups. [46]
Community testing stopped on March 13, 2020. On May 28, the new NHS Test and Trace service was launched, after the peak of the epidemic had passed and after the first easing of the national lockdown had been implemented. [47] During the peak of the epidemic, the government attempted to scale up testing capacity but failed. [48] In late April, it was reported that the government met its target of carrying out 100,000 tests a day, but the methods used for reporting artificially inflated the numbers. [49]
The lack of a clear national strategy based on transparent epidemiological evidence and the lack of clear official communications, including on the number of tests performed, mark a failure to prepare for the epidemic. The reliance on self-isolation while pubs, offices, and major events remained open; the delay in implementing a national lockdown; the decision to stop community testing mid-March coupled with the late launch of the Test and Trace service late May constitute a failure by the UK government to take strong action to contain and control the spread of the virus. The lack of sufficient PPE for NHS workers and people in social care homes, and of ventilators for seriously ill patients, represents a failure to treat and control the epidemic.
Obligation 4: Provide education and access to information concerning health
Two obligations can be distinguished in relation to information. First, states must report on their progress to fulfill the right to health and publish reliable data on indicators such as incidence and mortality. Second, states have a duty to ensure that health information of sufficient quality is circulated to the public. [50]
Data about COVID-19 are questionable everywhere, including the UK. It is impossible to know the true incidence rate because some infections produce few or no symptoms. While the effects of the disease range from mild to severe to fatal, the UK was not initially testing people outside hospitals. Even calls to NHS 111, the national helpline, from people with COVID-19 symptoms were not systematically registered. Deaths due to COVID-19 outside hospitals were not routinely reported by government agencies, therefore underestimating the death toll. Deaths in hospitals that are attributed to COVID-19 among patients with underlying conditions lack clarity because the cause of death may not necessarily be COVID-19. The curve of deaths may also not be reliable because deaths were being reported at the time of registration, not in relation to the date of death. Reporting times vary between health centers. [51] Without reliable data, public policy cannot be properly informed. For these reasons, scientists recommend relying on the number of excess deaths for international comparisons of COVID-19-related deaths. [52]
The WHO director-general used the term “infodemic” to describe an excessive amount of information about the COVID-19 pandemic, which makes it difficult for the general public to identify reliable information and act responsibly. [53] The “infodemic” has caused both health-related and economic damages in the UK, partly because the government failed to prevent and control misinformation. For instance, some conspiracy theories fueled the belief that SARS-CoV-2 was made in a lab, or that it was spread through the 5G communications network, resulting in attacks on telecom engineers and the burning of cell phone towers. [54] Official communication on the country’s testing capacity was unclear, with numbers on testing capacity artificially inflated and the number of COVID-19 cases deflated. [55] Communication around herd immunity sent the wrong signals to the population, days before the government announced that everyone should voluntarily self-isolate. These examples show a failure of the UK government to uphold its duty to provide clear and reliable information so that members of the public had the necessary tools to make informed choices regarding their health and to protect the health of others.
Obligation 5: Provide appropriate training for health personnel
A key function of the health system is to train its workers and ensure that they are ready to handle outbreaks of diseases. [56] The situation late March 2020 in the UK, about one month after the start of the COVID-19 outbreak in the country, showed inadequate training of health workers to respond to such an emergency. [57]
In 2016, Exercise Cygnus, a simulation exercise, was conducted to evaluate the capacity of the NHS in the event of a pandemic. The final report was kept secret, with some commentators arguing that it would have revealed that the NHS was unprepared for a pandemic. [58] It culminated in a freedom of information request from an NHS doctor in April 2020. [59] The report was eventually leaked to the Guardian, which published it in the interest of the public on May 7. [60]
One of the report’s key findings was that “the UK’s preparedness and response, in terms of its plans, policies and capability, [was] not sufficient to cope with the extreme demands of a severe pandemic that [would] have a nationwide impact across all sectors.” [61] In addition, the report identified a need to develop a “methodology for assessing social care capacity and surge capacity during a pandemic,” as well as to examine “the possibility of expanding social care real-estate and staffing capacity.” [62] These recommendations were not communicated to key stakeholders, as the Chief Executive of Care England testified. [63]
The lack of appropriate training for health personnel also comes from a more structural issue within the UK’s health system. The social care sector in England, as well as the NHS, have seen drastic financial cuts for the past ten years, in addition to privatization. Working conditions for social care workers are deplorable, with low pay and zero-hours contracts. [64] Junior doctors also work very long hours. The social care sector is now almost exclusively in the private sector and isolated from the NHS. Because of these structural issues, the current public health crisis has further amplified the problems faced by a tired and deficient workforce. [65]
The state’s failure to implement the recommendations from the pandemic preparedness exercise, its efforts to keep the final report confidential, and the fragmentation and privatization of the NHS and social care sector over the past ten years, mark a collective failure to comply with the obligation to train health workers and prepare the health sector to respond to outbreaks of diseases. [66]
This brief examination of the UK government’s early response to COVID-19 reveals four types of consequences from the failure to respect, protect, and fulfill the right to health, as illustrated in Table 1. The first type concerns direct health consequences—for example, people dying as a result of COVID-19, people losing family members to the disease, or people left with long-term sequelae after surviving an infection with the virus. The second concerns direct economic consequences—for example, people losing their jobs or homes, people being dragged into poverty, or children being unable to access school meals. The third category includes indirect health consequences, particularly for non-COVID patients with another serious health conditions. For instance, the diagnosis, management, and follow-up of cancer patients was greatly affected, which will almost inevitably lead to worse cancer outcomes. [67] This category also includes consequences stemming from the psychological impact of the lockdown. Finally, the fourth type concerns indirect economic consequences—for example, people bearing the costs of more expensive treatment for pre-existing health conditions or the loss of their job due to health complications after a late cancer diagnosis. Other indirect consequences stemming from the government’s failure to provide reliable information about the virus include property damage to 5G towers. All of these consequences had an impact on one another; for example, people dragged into poverty due to the pandemic are more likely to experience worse health later in life, since poverty is a social determinant of health. [68]
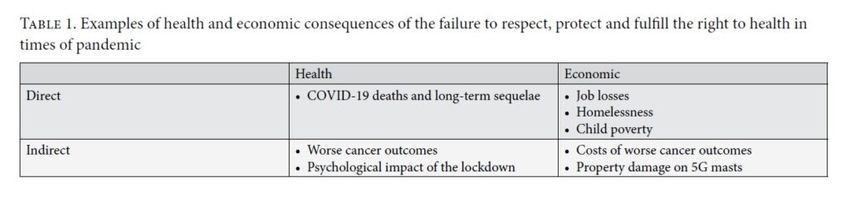 |
While late action from the government is to blame, the inadequacy of national responses worldwide also brings under scrutiny the utility and appropriateness of international legal provisions regarding the right to health. Are these legal texts adequate to address preparedness, surveillance, and promotion of the right to health for everyone in times of pandemic?
The international legal framework on pandemics and the right to health
We find that references to pandemics or public health crises are limited in human rights law documents.
General Comment 14 encourages “the creation of a system of urgent medical care in cases of accidents, epidemics and similar health hazards, and the provision of disaster relief and humanitarian assistance in emergency situations.” [69] This is supplemented by the European Committee on Social Rights’ Statement of Interpretation on the Right to Protection of Health in Times of Pandemic, which outlines states’ obligations to test, trace, and impose measures of physical distancing or lockdown and to ensure the availability of hospital beds, intensive care units, and PPE for health workers. [70] Of particular relevance to the UK, the European Committee on Social Rights emphasizes the need for states to act as soon as preliminary scientific evaluation indicates reasonable grounds for concern regarding potentially dangerous effects of a virus or other factors on human health. [71] The UK’s delay in implementing a national lockdown and the confusion generated by the government’s communications concerning the official public health strategy reveal the importance of such obligations. They all point toward states’ duty to prepare adequately for a pandemic and to ensure the availability of sufficient material and human resources to treat a large number of patients at any one time.
Further, international human rights law points toward a “collective responsibility” of the international community with regard to outbreaks of infectious diseases. [72] In the present context, the Committee on Economic, Social and Cultural Rights clarified that international cooperation means sharing medical equipment and best practices to combat the virus, sharing knowledge for the development of a vaccine, and engaging in joint action to minimize the economic and social impacts of the public health crisis. [73] International cooperation around COVID-19 seems to have been weak at first, with, for instance, Italy’s call for help met with silence from other European countries. [74] The President of the European Commission, the UN Secretary-General, and the WHO called for solidarity among countries. [75] At the global level, many countries contributed to the COVID-19 Solidarity Response Fund. [76] However, this generosity was soon overshadowed by the announcement from President Trump that the United States would withdraw its funding to WHO. International cooperation has not been satisfactory, and the pandemic response has emerged as a turf war between different polities, with some country leaders blaming China or banning exports of medicine. [77]
We did not find further mentions of pandemics or public health emergencies in international human rights instruments. The closest we found was the inclusion in these instruments of a duty for states to engage in international cooperation and to create systems of urgent care. However, as illustrated by the example of the UK in the COVID-19 pandemic, many other issues require attention, such as the training of medical staff in infection prevention and control, the prompt response and planning by the government as soon as scientific evidence becomes available, the transparency of the government’s response based on scientific evidence, the accuracy of data collected and communicated, the provision of continuing care for everyone (including patients with conditions other than COVID-19), the management of intensive care services, and the regulation of food supplies, to name but a few. In this regard, the Statement of Interpretation on the Right to Protection of Health in Times of Pandemic from the European Committee on Social Rights constitutes an encouraging development, because it extends states’ obligations to include the adoption of public health measures to prevent, contain, and control the spread of viruses, as well as to treat the diseases they cause.
The binding 2005 International Health Regulations and the non-binding 2011 Pandemic Influenza Preparedness Framework are key international documents that apply to all WHO member states with regard to preparing for outbreaks of infectious diseases. [78] While they are of critical importance from a public health perspective, and despite referring to human rights principles, we argue that they are not sufficient for the protection of the right to health in times of pandemic because they do not propose a rights-based approach to public health emergencies. They should, however, inform future development of the right to health.
Recommendations
International human rights law on the right to health needs updating. The inadequacy of responses to the COVID-19 pandemic that should have protected and safeguarded the right to health signals an urgent need for the firm grounding of pandemic preparedness plans in human rights principles. The suitability of human rights instruments in the context of a health emergency also needs urgent reviewing.
The example of the UK shows that the public health response must explicitly address vulnerable groups in the general population—including older patients with chronic conditions, ethnic minorities, non-COVID patients with another serious health condition (such as cancer), people with mental or physical disabilities, people living in deprived areas and crowded households—to ensure universal access to health services and facilities.
Addressing human rights is especially needed during lockdown, because such measures disproportionately affect vulnerable groups, including women experiencing abuse. a href="#_edn79" name="_ednref79">[79] Early studies suggest that people in BAME communities are more likely to die of COVID-19 than white people. [80] This may be due to the increased pressure faced by BAME doctors and nurses to see infected patients in settings without PPE, the fact that people from ethnic minorities are more likely to live in severely affected areas, and BAME individuals’ greater likelihood of having underlying health conditions. [81] Either way, states must implement measures that will protect groups at higher risk of dying from the disease, including those in social care homes.
Protecting vulnerable groups extends beyond access to health care. In the UK, many households are now affected economically by the crisis, as observed with the increased demand on food banks.
Experience in the UK also shows the need for a clear national strategy from the outset, as soon as a risk is reasonably identified through scientific evidence. Political action must be prompt, based on scientific evidence, transparent, and communicated clearly to the population. A soft approach like the one adopted by the UK in the weeks preceding the lockdown, where private actors with economic power remained in charge of deciding whether people should travel to work and whether events would be maintained, should be avoided.
Further, communication around the pandemic necessitates a minimum level of control by the state, especially in times of mass misinformation and spread of fake news through social media channels. While it is important to maintain freedom of the press and freedom of expression, the state must guide the public toward reliable sources of information that are transparent and based on science. Data on the virus must be published using a clear method so as not to mislead the public, as pointed out by the UK Statistics Authority when criticizing the misuse of statistics by the Secretary of State for Health on June 2, 2020. [82]
Because in the UK, as in many other countries, health workers initially lacked PPE in sufficient number and quality, the provision of essential medical goods must be at the forefront of a state’s response to a pandemic—without, however, depriving other countries of such goods.
Based on the UK example of a state’s response to COVID-19, we call on international experts in human rights, health systems, infectious diseases, non-communicable diseases, emergency care, and humanitarian disasters to develop a robust framework of protections that would be applicable in times of pandemic. This framework should include the following:
- A universal right to access urgent medical care on a non-discriminatory basis
- A universal right to screening, prompt diagnosis, treatment, and continuing care for non-communicable diseases, on a non-discriminatory basis, in order to continue progress towards Sustainable Development Goal 3.4, i.e. to reduce by one-third premature mortality for non-communicable diseases by 2030 (cancer, diabetes, heart diseases, and respiratory diseases)
- The duty of states to act promptly and prepare for a disease outbreak as soon as scientific evidence indicates reasonable grounds for concern regarding potentially dangerous effects of a virus or other factors on human health
- The duty of states to adopt a national response plan based on scientific evidence available to the public
- The duty of states to ensure accurate data collection and dissemination by public agencies or universities, without political interference
- The duty of states to publish disaggregated data that would help identify discrimination on grounds such as sex, ethnicity, and socioeconomic status
- The duty of states, using an intersectionality lens, to monitor risks of infection and access to health care among vulnerable groups
- The duty of states, in collaboration with WHO and social media platforms, to control the spread of misinformation, fake news, and rumors about viruses and the diseases they cause, including racial blame and victimization
- The duty of states to ensure the regular flow of food supplies everywhere in their territories, with particular attention to deprived households
- The duty of states to ensure that medical staff have the necessary resources to work, including PPE, disinfectant, and medical supplies of adequate quality relevant to the disease being treated
In addition, the right to health as enshrined in international human rights law should be updated to include the following provisions:
- A core minimum obligation to ensure access to emergency care on a non-discriminatory basis
- The duty of states to build and support robust and resilient health systems based on scientific evidence, on WHO’s six building blocks (governance, financing, workforce, products and technologies, information and research, and service delivery), and on human rights principles of non-discrimination, participation, accountability as well as the availability, accessibility, acceptability and quality framework
- The training of health and social care professionals in infection prevention and control, in both the public and private sectors
Such provisions could either be added to a revised version of General Comment 14 or be included in a new general comment on the right to health in times of pandemic. Regional human rights bodies such as the European Committee on Social Rights, the African Commission on Human and Peoples’ Rights, the Inter-American Commission on Human Rights, the Arab Human Rights Committee, and the South Asian Association for Regional Cooperation should adopt recommendations on the right to health in times of pandemic and consider including the above provisions.
Conclusion
The risk of pandemics from new viruses is likely to increase due to a growing world population, urbanization, and frequency of international travels, together with the presence of live animal markets in densely populated areas. The Statement on the Right to Health in Times of Pandemic from the European Committee on Social Rights builds on the robust international legal framework for the right to health and constitutes an encouraging basis to develop it further.
In this article, we observe the UK’s response to the COVID-19 pandemic and identify some issues that have emerged in such exceptional times. We argue that the right to health as enacted today is not sufficient to address these issues. The current international human rights framework is robust, but states’ obligations should be clarified so they can be adapted to public health measures in times of pandemic. At the same time, international public health documents to prepare for pandemics are not sufficient on their own to protect the right to health of everyone. We offer some recommendations to that effect.
Writing about issues as we witness them allows us to construct reliable historic memory. The COVID-19 pandemic has caused many deaths that could have been avoided had we been better prepared with strong rights-based provisions. These are essential lessons to be learned, and the human rights community has a crucial role to play to ensure that future responses to pandemics are grounded in human rights law.
We would like to thank members of the Economic and Social Rights Academic Network of the UK and Ireland for their valuable comments on earlier drafts of this article. We would also like to thank Dr Claire Lougarre for her detailed and in-depth comments that strengthened the legal analysis of this article.
Lisa Montel, LLM, is PhD candidate in the Cancer Survival Group, Department of Non-Communicable Disease Epidemiology at the London School of Hygiene and Tropical Medicine, and Research Associate in the Social Sciences and Law Faculty at the University of Bristol, UK.
Anuj Kapilashrami, MA, MSc, PhD, is Professor in Global Health Policy and Equity at the School of Health and Social Care at the University of Essex, Colchester, UK.
Michel P. Coleman, BA, BM, BCh, MSc, FFPH, is Professor of Epidemiology and Vital Statistics and Head of the Cancer Survival Group, Department of Non-Communicable Disease Epidemiology at the London School of Hygiene and Tropical Medicine, UK.
Claudia Allemani, MSc, PhD, FHEA, MFPH, is Associate Professor of Cancer Epidemiology in the Cancer Survival Group, Department of Non-Communicable Disease Epidemiology at the London School of Hygiene and Tropical Medicine, UK.
Please address correspondence to Lisa Montel. Email: lisa.montel@lshtm.ac.uk.
Competing interests: None declared.
[Source: Health and Human Rights Journal, Harvard T.H. Chan School of Public Health, Volume 22/2, December 2020, pp 227 – 242.
Available online in pdf format at: https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2469/2020/12/Montel.pdf]
References
[1] European Committee of Social Rights, Statement of Interpretation on the Right to Protection of Health in Times of Pandemic (2020).
[2] J. Bueno De Mesquita, C. Lougarre, L. Montel, and S. Sekalala, “The government’s response to COVID-19: How to further realise the right to health,” written evidence to the UK Parliament Committee of Human Rights, COV0195 (July 2020).
[3] United Nations Sustainable Development Group, COVID-19 and human rights: We are all in this together (April 2020); World Health Organization, Addressing human rights as key to the COVID-19 response (April 2020), p. 1; D. Puras, J. Bueno de Mesquita, L. Cabal, et al., “The right to health must guide responses to COVID-19,” Lancet 395/10241 (2020), pp. 1888–1890.
[4] R. Horton, “Offline: COVID-19 and the NHS—‘a national scandal,’” Lancet 395/10229 (2020), p. 1022; R. Horton, N. Alwan, M. Orcutt, et al., “Coronavirus modelling ‘must be made clear,’” Times (March 14, 2020); UK Parliament Joint Committee on Human Rights, Written evidence: The government’s response to COVID-19: Human rights implications, (2020). Available at https://www.committees.parliament.uk/work/218/the-governments-response-to-covid19-human-rights-implications/publications/written-evidence/?page=2.
[5] L. S. Vestergaard, J. Nielsen, L. Richter, et al., “Excess all-cause mortality during the COVID-19 pandemic in Europe: Preliminary pooled estimates from the EuroMOMO network, March to April 2020,” Eurosurveillance 25/26 (2020).
[6] European Social Charter, 529 U.N.T.S. 89 (1961), art. 11; International Covenant on Economic, Social and Cultural Rights, G.A. Res. 2200A (XXI) (1966), art. 12.
[7] Committee on Economic Social and Cultural Rights, General Comment No. 14: The Right to the Highest Attainable Standard of Health, UN Doc. E/C12/2000/4 (2000), paras. 43–44.
[8] G. Backman, P. Hunt, R. Khosla, et al., “Health systems and the right to health: An assessment of 194 countries,” Lancet 372/9655 (2008), pp. 2047–2085.
[9] International Covenant on Economic, Social and Cultural Rights, G.A. Res. 2200A (XXI) (1966).
[10] Convention on the Elimination of All Forms of Discrimination against Women, G.A. Res. 34/180 (1979), art. 12; Convention on the Rights of Persons with Disabilities, G.A. Res. 61/106 (2007), art. 25; Convention on the Rights of the Child, G.A. Res. 44/25 (1989), art. 24.
[11] International Covenant on Economic, Social and Cultural Rights, G.A. Res. 2200A (XXI) (1966), art. 2(1).
[12] Committee on Economic, Social and Cultural Rights (2000, see note 7), paras. 43–44.
[13] J. Bedford, D. Enria, J. Giesecke, et al., “COVID-19: Towards controlling of a pandemic,” Lancet 395/10229 (2020), pp. 1015–1018; A. Pollock, P. Roderick, K. K. Cheng, et al., “Covid-19: Why is the UK government ignoring WHO’s advice?” BMJ 369 (2020), m1284; World Health Organization, Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) (January 30, 2020); World Health Organization, Responding to community spread of COVID-19: Interim guidance, (March 7, 2020); World Health Organization, Pandemic influenza risk management: WHO interim guidance (2013).
[14] World Health Organization, “Novel coronavirus—China, disease outbreak news: Update” (January 12, 2020).
[15] Ibid.
[16] World Health Organization (January 30, 2020, see note 13).
[17] Ibid.
[18] Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584(7821): 430-6.
[19] Public Health England, “COVID-19: Review of disparities in risks and outcomes” (June 2020); Deeny S, Dunn P. The devastating impact of covid-19 on social care in England. BMJ Opinion; 2020.
[20] NHS England, “Advice on how to establish a remote ‘total triage’ model in general practice using online consultations” (April 2020).
[21] NHS England, “NHS improvement, important and urgent: Next steps on NHS response to COVID-19” (March 17, 2020).
[22] Health Foundation, “COVID-19: Five dimensions of impact” (April 29, 2020).
[23] P. F. Stahel, “How to risk-stratify elective surgery during the COVID-19 pandemic?” Patient Safety in Surgery 14 (2020), p. 8.
[24] National Health Service, “Clinical guide for the management of noncoronavirus patients requiring acute treatment: Cancer” (March 23, 2020); National Health Service, “Clinical guide for the management of essential cancer surgery for adults during the coronavirus pandemic” (April 7, 2020); National Health Service, “Clinical guide to surgical prioritisation during the coronavirus pandemic” (April 11, 2020).
[25] NHS England, “Advice to trusts on maintaining cancer treatment during the COVID-19 response” (March 30, 2020).
[26] K. Roberts, “Over 2 million people waiting for cancer screening, tests and treatments,” Cancer Research UK (June 1, 2020).
[27] D. Jones, R. D. Neal, S. R. G. Duffy, et al., “Impact of the COVID-19 pandemic on the symptomatic diagnosis of cancer: The view from primary care,” Lancet Oncology 21/6 (2020), pp. 748–750.
[28] Cancer Research UK, “Coronavirus and cancer: Latest updates” (March 19, 2020).
[29] International Covenant on Economic, Social and Cultural Rights, G.A. Res. 2200A (XXI) (1966), art. 11; Committee on Economic, Social and Cultural Rights, General Comment No. 12: The Right to Adequate Food, UN Doc. E/C12/1999/5 (1999).
[30] Public Health England, “Guidance for food businesses on coronavirus (COVID-19)” (March 25, 2020).
[31] Food Standards Agency, “Guidance for consumers on coronavirus (COVID-19) and food” (April 17, 2020).
[32] UK Statutory Instruments, The Competition Act 1998 (Groceries) (Coronavirus) (Public Policy Exclusion) Order 2020, No. 369 (March 27, 2020).
[33] UK Public General Acts, Coronavirus Act 2020, c.7 (March 25, 2020).
[34] H. Lock, “COVID-19 lockdowns are sparking a hunger crisis in the UK,” Global Citizen (April 22, 2020); Power M, Doherty B, Pybus K, Pickett K. How COVID-19 has exposed inequalities in the UK food system: The case of UK food and poverty. Emerald Open Research 2020; 2: 11.
[35] World Health Organization (2020, 2013, see note 13).
[36] Coronavirus (COVID-19) in the UK (2020). Available at https://coronavirus.data.gov.uk.
[37] Department of Health and Social Care, “Coronavirus: Action plan” (March 3, 2020).
[38] G. Parker, J. Pickard, and L. Hughes, “UK’s chief scientific adviser defends ‘herd immunity’ strategy for coronavirus,” Financial Times (March 13, 2020).
[39] N. Ferguson, D. Laydon, G. Nedjati-Gilani, et al., “Report 9: Impact of non-pharmaceutical interventions (NPIs) to reduce COVID-19 mortality and healthcare demand,” Imperial College London (2020).
[40] Horton et al. (2020, see note 4); W. Hanage, “I’m an epidemiologist. When I heard about Britain’s ‘herd immunity’ coronavirus plan, I thought it was satire,” Guardian (March 15, 2020).
[41] UK Public General Acts (2020, see note 33); UK Statutory Instruments, The Health Protection (Coronavirus, Restrictions) (England) Regulations 2020, No. 350 (March 26, 2020).
[42] Pollock et al. (2020, see note 13); World Health Organization (2020), see note 13, Scally G, Jacobson B, Abbasi K. The UK’s public health response to covid-19. BMJ 2020; 369: m1932.
[43] Horton (2020, see note 4); J. P. Thomas, A. Srinivasan, C. S. Wickramarachchi, et al., “Evaluating the national PPE guidance for NHS healthcare workers during the COVID-19 pandemic,” Clinical Medicine 20/3 (2020), p. 242.
[44] F. Guarascio, “EU says Britain had chance to join ventilator procurement scheme,” Reuters (March 27, 2020).
[45] DJ. Hunter, “Covid-19 and the stiff upper lip: The pandemic response in the United Kingdom,” New England Journal of Medicine 382/16 (2020), p. e31.
[46] Health Foundation, “What has been the impact of COVID-19 on care homes and the social care workforce?” (2020); Deeny S, Dunn P. The devastating impact of covid-19 on social care in England. BMJ Opinion; 2020.
[47] Department of Health and Social Care, “Government launches NHS Test and Trace service” (May 27, 2020); A. Pollock, P. Roderick, K. K. Cheng, et al., “Covid-19: Why is the UK government ignoring WHO’s advice?” BMJ 369 (2020), m1284; World Health Organization, Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV) (January 30, 2020).
[48] “Health Secretary sets out plan to carry out 100,000 coronavirus tests a day” (April 2, 2020); “Coronavirus (COVID-19): Scaling up testing programmes” (April 4, 2020); “UK pays £16 million for coronavirus tests that don’t work,” Independent (April 17, 2020).
[49] UK Statistics Authority, “Sir David Norgrove response to Matt Hancock regarding the Government’s COVID-19 testing data” (June 2, 2020); Department of Health and Social Care, Public Health England, “Number of coronavirus (COVID-19) cases and risk in the UK: the latest number of coronavirus (COVID-19) cases and risk level in the UK” (2020). Available at https://www.gov.uk/guidance/coronavirus-covid-19-information-for-the-public.
[50] Committee on Economic, Social and Cultural Rights (2000, see note 7); Office of the United Nations High Commissioner for Human Rights and World Health Organization, Fact sheet no. 31: The right to health (2008). Available at https://www.ohchr.org/Documents/Publications/Factsheet31.pdf.
[51] M. P. Coleman, V. Di Carlo, J. R. Ashton, et al., “Reliable, real-world data on excess mortality are required to assess the impact of covid-19,” BMJ Opinion (May 7, 2020).
[52] Ibid.; D. A. Leon, V. M. Shkolnikov, L. Smeeth, et al., “COVID-19: A need for real-time monitoring of weekly excess deaths,” Lancet 395/10234 (2020), p. e81.
[53] World Health Organization, “WHO Director-General speech: Munich Security Conference 2020” (2020).
[54] J. Waterson and A. Hern, “At least 20 UK phone masts vandalised over false 5G coronavirus claims,” Guardian (April 6, 2020).
[55] UK Statistics Authority (see note 49).
[56] World Health Organization, “WHO addresses parliamentarians on COVID-19 pandemic” (April 28, 2020).
[57] Horton (2020, see note 4).
[58] “If ministers fail to reveal 2016 flu study they ‘will face court,’” Observer (April 26, 2020).
[59] Leigh Day, “Cygnus Report legal challenge update” (April 28, 2020).
[60] D. Pegg, R. Booth, and D. Conn, “Revealed: The secret report that gave ministers warning of care home coronavirus crisis,” Guardian (May 7, 2020).
[61] Public Health England, “Exercise Cygnus report tier one command post exercise pandemic influenza 18 to 20 October 2016” (2017), p. 6.
[62] Ibid, p. 31.
[63] Pegg et al. (see note 60).
[64] A. Pollock, L. Clements, L. Harding-Edgar, “Covid-19: Why we need a national health and social care service,” BMJ 369 (2020), p. m1465.
[65] Ibid.
[66] World Health Organization (2013, see note 13).
[67] Jones et al. (see note 27); Hamilton W. Cancer diagnostic delay in the COVID-19 era: what happens next? The Lancet Oncology 2020; 21(8): 1000-2; Maringe C, Spicer J, Morris M, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. The Lancet Oncology 2020; 21(8): 1023-34.
[68] Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. The Lancet 2008; 372(9650): 1661-9.
[69] Committee on Economic, Social and Cultural Rights (2000, see note 7), para. 16.
[70] European Committee of Social Rights (see note 1), p. 3.
[71] Ibid, p. 4.
[72] Committee on Economic Social and Cultural Rights (2000, see note 7); Committee on Economic, Social and Cultural Rights, Statement on the coronavirus disease (COVID-19) pandemic and economic, social and cultural rights, UN Doc. E/C12/2020/1 (2020).
[74] D. Herszenhorn, C. Paun, and J. Deutsch, “Europe fails to help Italy in coronavirus fight,” Politico (March 5, 2020); Sekalala S, Forman L, Habibi R, Meier BM. Health and human rights are inextricably linked in the COVID-19 response. BMJ Global Health 2020; 5(9): e003359.
[75] P. Tamma and L. Bayer, “Von der Leyen calls for ‘tangible’ solidarity on €100B jobs scheme,” Politico (April 2, 2020); World Health Organization. Addressing Human Rights as Key to the COVID-19 Response, 2020; Guterres A. This is, above all, a human crisis that calls for solidarity. 2020. https://www.un.org/en/un-coronavirus-communications-team/above-all-human-crisis-calls-solidarity [Accessed on 29 October 2020].
[76] World Health Organization, “Coronavirus disease (COVID-19) donors and partners: WHO says thank you!” (2020). Available at https://www.who.int/emergencies/diseases/novel-coronavirus-2019/donors-and-partners/funding.
[77] A. Liu, “Blaming China for coronavirus isn’t just dangerous. It misses the point,” Guardian (April 10, 2020); Department of Health and Social Care, “Crucial medicines protected for coronavirus (COVID-19) patients,” (March 20, 2020); “France ignores EU calls to lift export bans on Covid-19 drugs,” France 24 (April 23, 2020).
[78] World Health Organization (2013, see note 8); World Health Organization, International Health Regulations (2005).
[79] J. S. Chandan, J. Taylor, C. Bradbury-Jones, et al., “COVID-19: A public health approach to manage domestic violence is needed,” Lancet Public Health 5/6 (2020); Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584(7821): 430-6.
[80] A. Kapilashrami and K. Bhui, “Mental health and COVID-19: Is the virus racist?” British Journal of Psychiatry 217/2 (2020), pp. 405–407; Williamson EJ, Walker AJ, Bhaskaran K, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020; 584(7821): 430-6.
[81] T. Kirby, “Evidence mounts on the disproportionate effect of COVID-19 on ethnic minorities,” Lancet Respiratory Medicine 8/6 (2020).
[82] UK Statistics Authority (see note 49).

